Our website is made possible by displaying online advertisements to our visitors.
Please consider supporting us by disabling your ad blocker.
Allergic bronchopulmonary aspergillosis
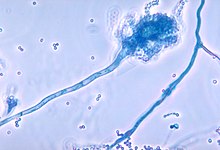
Allergic bronchopulmonary aspergillosis (ABPA) is a condition characterised by an exaggerated response of the immune system (a hypersensitivity response) to the fungus Aspergillus (most commonly Aspergillus fumigatus). It occurs most often in people with asthma or cystic fibrosis.[1] Aspergillus spores are ubiquitous in soil and are commonly found in the sputum of healthy individuals. A. fumigatus is responsible for a spectrum of lung diseases known as aspergilloses.[4]
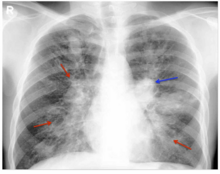
ABPA causes airway inflammation, leading to bronchiectasis—a condition marked by abnormal dilation of the airways. Left untreated, the immune system and fungal spores can damage sensitive lung tissues and lead to scarring.[5]
The exact criteria for the diagnosis of ABPA are not agreed upon. Chest X-rays and CT scans, raised blood levels of IgE and eosinophils, immunological tests for Aspergillus together with sputum staining and sputum cultures can be useful. Treatment consists of corticosteroids and antifungal medications.[2]
- ^ a b c Cite error: The named reference
Kousha2011was invoked but never defined (see the help page). - ^ a b c d e f Sisodia, Jitendra; Bajaj, Tushar (August 8, 2023). "Allergic Bronchopulmonary Aspergillosis". StatPearls Publishing. PMID 31194469. Retrieved October 14, 2023.
- ^ "Aspergillosis Statistics — Aspergillosis — Types of Fungal Diseases — Fungal Diseases". CDC. December 5, 2019. Retrieved October 14, 2023.
- ^ Bandres, Maria V.; Modi, Pranav; Sharma, Sandeep (August 8, 2023). "Aspergillus Fumigatus". StatPearls Publishing. PMID 29494071. Retrieved October 14, 2023.
- ^ Abuzneid, Yousef S.; Yaghi, Yasmine; Madia, Arein; Salhab, Nataly; Amro, Naser; Abukhalaf, Sadi A.; Kharraz, Mohammad (2021). "Misdiagnosis of persistent asthma of a patient suffering from acute bronchopulmonary aspergillosis (ABPA)". Annals of Medicine & Surgery. 68. Ovid Technologies (Wolters Kluwer Health). doi:10.1016/j.amsu.2021.102696. ISSN 2049-0801. PMC 8361028.
Previous Page Next Page
داء الرشاشيات القصبي الرئوي الأرجي Arabic Allergische bronchopulmonale Aspergillose German Aspergilosis broncopulmonar alérgica Spanish Aspergillose bronchopulmonaire allergique French Asperxilose broncopulmonar alérxica GL Aspergillosi broncopolmonare allergica Italian アレルギー性気管支肺アスペルギルス症 Japanese ବ୍ରୋଙ୍କୋପଲମୋନାରୀ ଆସ୍ପର୍ଗିଲୋସିସ ଆଲର୍ଜି OR Alergijska bronhopulmonalna aspergiloza SL