Our website is made possible by displaying online advertisements to our visitors.
Please consider supporting us by disabling your ad blocker.
Benzodiazepine dependence
| Benzodiazepine dependence | |
|---|---|
| Other names | Benzodiazepine addiction |
 | |
| Lorazepam (Ativan) tablets | |
| Specialty | Addiction Medicine |
| Complications | Benzodiazepine overdose |
Benzodiazepine dependence (BZD dependence) defines a situation in which one has developed one or more of either tolerance, withdrawal symptoms, drug seeking behaviors, such as continued use despite harmful effects, and maladaptive pattern of substance use, according to the DSM-IV. In the case of benzodiazepine dependence, the continued use seems to be typically associated with the avoidance of unpleasant withdrawal reaction rather than with the pleasurable effects of the drug.[1] Benzodiazepine dependence develops with long-term use, even at low therapeutic doses,[2] often without the described drug seeking behavior and tolerance.[3][4]
Addiction consists of people misusing or craving the drug, not to relieve withdrawal symptoms, but to experience its euphoric or intoxicating effects. It is necessary to distinguish between addiction to and abuse of benzodiazepines, and physical dependence on them. The increased GABA inhibition on the neural systems caused by benzodiazepines is counteracted by the body's development of tolerance to the drug's effects; the development of tolerance occurs as a result of neuroadaptations, which result in decreased GABA activity and increased excitability of the glutamate system; these adaptations occur as a result of the body trying to overcome the central nervous system depressant effects of the drug to restore homeostasis. When benzodiazepines are stopped, these neuroadaptations are "unmasked" leading to hyper-excitability of the nervous system and the appearance of withdrawal symptoms.[5]
Therapeutic dose dependence is the largest category of people dependent on benzodiazepines. These individuals typically do not escalate their doses to high levels and generally use their medication as intended by their prescriber. Smaller groups include patients escalating their dosage to higher levels and drug misusers as well. Tolerance develops within days or weeks to the anticonvulsant, hypnotic, muscle relaxant and after 4 months there is little evidence that benzodiazepines retain their anxiolytic properties.[6] Some authors, however, disagree and feel that benzodiazepines retain their anxiolytic properties.[7] Long-term benzodiazepine treatment may remain necessary in certain clinical conditions.[8]
Numbers of benzodiazepine prescriptions have been declining, due primarily to concerns of dependence. In the short term, benzodiazepines can be effective drugs for acute anxiety or insomnia. With longer-term use, other therapies, both pharmacological and psychotherapeutic, become more effective. This is in part due to the greater effectiveness over time of other forms of therapy, and also due to the eventual development of pharmacological benzodiazepine tolerance.[9][10]
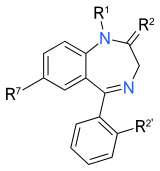
| Benzodiazepines |
|---|
 |
- ^ de Wit H, Griffiths RR (June 1991). "Testing the abuse liability of anxiolytic and hypnotic drugs in humans". Drug and Alcohol Dependence. 28 (1): 83–111. doi:10.1016/0376-8716(91)90054-3. PMID 1679388.
- ^ Nutt DJ (1 January 1986). "Benzodiazepine dependence in the clinic: reason for anxiety". Trends Neurosci. 7: 457–460. doi:10.1016/0165-6147(86)90420-7. Archived from the original on 9 March 2014. Retrieved 21 December 2012.
- ^ Marriot S, Tyrer P (August 1993). "Benzodiazepine dependence. Avoidance and withdrawal". Drug Safety. 9 (2): 93–103. doi:10.2165/00002018-199309020-00003. PMID 8104417. S2CID 8550990. Archived from the original on 18 February 2024. Retrieved 18 February 2024.
- ^ O'brien CP (2005). "Benzodiazepine use, abuse, and dependence". J Clin Psychiatry. 66 (Suppl 2): 28–33. PMID 15762817.
- ^ Cite error: The named reference
Allison-2003was invoked but never defined (see the help page). - ^ Cite error: The named reference
Committee on the Review of Medicines 910–2was invoked but never defined (see the help page). - ^ Cite error: The named reference
asapdacgwas invoked but never defined (see the help page). - ^ Cloos JM, Ferreira V (January 2009). "Current use of benzodiazepines in anxiety disorders". Current Opinion in Psychiatry. 22 (1): 90–95. doi:10.1097/YCO.0b013e32831a473d. PMID 19122540. S2CID 20715355.
- ^ Puri BK, Tyrer P (28 August 1998). "Clinical psychopharmacology". Sciences Basic to Psychiatry (2nd ed.). Churchill Livingstone. pp. 155–157. ISBN 978-0-443-05514-0. Retrieved 2009-07-11.[permanent dead link]
- ^ Longo LP, Johnson B (April 2000). "Addiction: Part I. Benzodiazepines--side effects, abuse risk and alternatives". Am Fam Physician. 61 (7): 2121–8. PMID 10779253. Archived from the original on 2008-05-12. Retrieved 2009-07-17.
Previous Page Next Page
اعتماد على البنزوديازيبين Arabic Psychische und Verhaltensstörungen durch Sedativa oder Hypnotika German Dependencia de las benzodiazepinas Spanish وابستگی به بنزودیازپینها FA Dipendenza da benzodiazepine Italian ベンゾジアゼピン依存症 Japanese Dependência de benzodiazepina Portuguese การติดยาเบ็นโซไดอาเซพีน Thai Benzodiazepin bağımlılığı Turkish Nghiện benzodiazepine VI


