Our website is made possible by displaying online advertisements to our visitors.
Please consider supporting us by disabling your ad blocker.
Fat embolism syndrome
| Fat embolism syndrome | |
|---|---|
| Other names | Fat embolism |
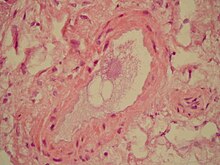 | |
| Microscopic section of the lungs showing a blood vessel with fibrinoid material and an empty space indicative of the presence of lipid dissolved during the staining process. Haematoxylin and eosin stain | |
| Specialty | Orthopedics, traumatology, pulmonology, intensive care medicine |
| Symptoms | Petechial rash, decreased level of consciousness, shortness of breath[1] |
| Complications | Personality changes, seizures, [2] Vessel blockage |
| Usual onset | Within 24 hours[1] |
| Causes | Bone fracture, pancreatitis, bone marrow transplant, liposuction[3] |
| Diagnostic method | Based on symptoms[2] |
| Differential diagnosis | Pulmonary embolism, pneumonia[2] |
| Prevention | Early stabilization of long bone fractures |
| Treatment | Supportive care[4] |
| Prognosis | 10% risk of death[2] |
| Frequency | Rare[4] |
Fat embolism syndrome occurs when fat enters the blood stream (fat embolism) and results in symptoms.[1] Symptoms generally begin within a day.[1] This may include a petechial rash, decreased level of consciousness, and shortness of breath.[1] Other symptoms may include fever and decreased urine output.[2] The risk of death is about 10%.[2]
Fat embolism most commonly occurs as a result of fractures of bones such as the femur or pelvis.[3][1] Other potential causes include pancreatitis, orthopedic surgery, bone marrow transplant, and liposuction.[3][2] The underlying mechanism involves widespread inflammation.[3] Diagnosis is based on symptoms.[2]
Treatment is mostly supportive care.[4] This may involve oxygen therapy, intravenous fluids, albumin, and mechanical ventilation.[2] While small amounts of fat commonly occur in the blood after a bone fracture,[3] fat embolism syndrome is rare.[4] The condition was first diagnosed in 1862 by Zenker.[1]
- ^ a b c d e f g Akhtar, S (September 2009). "Fat embolism". Anesthesiology Clinics. 27 (3): 533–50, table of contents. doi:10.1016/j.anclin.2009.07.018. PMID 19825491.
- ^ a b c d e f g h i Laurence, Knott (19 February 2014). "Fat embolism syndrome". patient.info. Archived from the original on 1 December 2017. Retrieved 14 March 2018.
- ^ a b c d e Adeyinka, A; Pierre, L (2020). "Fat Embolism". StatPearls. PMID 29763060.
- ^ a b c d Fukumoto, LE; Fukumoto, KD (September 2018). "Fat Embolism Syndrome". The Nursing Clinics of North America. 53 (3): 335–347. doi:10.1016/j.cnur.2018.04.003. PMID 30100000. S2CID 51969468.
Previous Page Next Page


