
Back التهاب الكبد الكحولي Arabic Hepatitis alcohòlica Catalan ھەوکردنی جگەری کحولی CKB Hepatitis alcohólica Spanish Alkoholihepatiitti Finnish Hépatite alcoolique aiguë French Hepatitis alkoholik ID Epatite alcolica Italian 알코올성 간염 Korean Alkoholiskais hepatīts Latvian/Lettish
| Alcoholic hepatitis | |
|---|---|
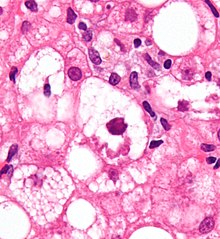 | |
| Micrograph showing a Mallory body, a histopathologic finding associated with alcoholic hepatitis. H&E stain. | |
| Specialty | Gastroenterology |
| Complications | Cirrhosis, kidney failure, confusion, drowsiness and slurred speech (hepatic encephalopathy), ascites, enlarged veins (varices)[1] |
| Risk factors | Sex, obesity, genetic factors, race and ethnicity, binge drinking[1] |
Alcoholic hepatitis is hepatitis (inflammation of the liver) due to excessive intake of alcohol.[2] Patients typically have a history of at least 10 years of heavy alcohol intake, typically 8–10 drinks per day.[3] It is usually found in association with fatty liver, an early stage of alcoholic liver disease, and may contribute to the progression of fibrosis, leading to cirrhosis. Symptoms may present acutely after a large amount of alcoholic intake in a short time period, or after years of excess alcohol intake. Signs and symptoms of alcoholic hepatitis include jaundice (yellowing of the skin and eyes), ascites (fluid accumulation in the abdominal cavity), fatigue and hepatic encephalopathy (brain dysfunction due to liver failure).[3] Mild cases are self-limiting, but severe cases have a high risk of death. Severity in alcoholic hepatitis is determined several clinical prediction models such as the Maddrey's Discriminant Function and the MELD score.
Severe cases may be treated with glucocorticoids with a response rate of about 60%. The condition often comes on suddenly and may progress in severity very rapidly.
- ^ a b "Alcoholic hepatitis". mayoclinic.org. Mayo Clinic. Retrieved June 5, 2022.
- ^ "Alcoholic liver disease: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2 January 2017.
- ^ a b Im, Gene Y. (February 2019). "Acute Alcoholic Hepatitis". Clinics in Liver Disease. 23 (1): 81–98. doi:10.1016/j.cld.2018.09.005. PMID 30454835. S2CID 53873388.