
Back اعتلال دماغي كبدي Arabic Hepatik ensefalopatiya AZ Encefalopatia hepàtica Catalan Hepatisk encefalopati Danish Hepatische Enzephalopathie German Hepata encefalopatio EO Encefalopatía hepática Spanish انسفالوپاتی کبدی FA Hepaattinen enkefalopatia Finnish Encéphalopathie hépatique French
| Hepatic encephalopathy | |
|---|---|
| Other names | Portosystemic encephalopathy, hepatic coma,[1] coma hepaticum |
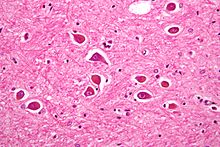 | |
| Micrograph of Alzheimer type II astrocytes, as may be seen in hepatic encephalopathy | |
| Specialty | Gastroenterology |
| Symptoms | Altered level of consciousness, mood changes, personality changes, movement problems[2] slurred speech, Sleep problems, Anxiety or irritability, Muscle twitches (myoclonus), Difficulty concentrating or short attention span, Flapping hand motion (asterixis), Reduced alertness, Cognitive impairment (confused thinking or judgment).[3] |
| Complications | hepatic coma.[3] |
| Types | Acute, recurrent, persistent[4] |
| Causes | Liver failure[2] |
| Risk factors | Infections, GI bleeding, constipation, electrolyte problems, certain medications[5] |
| Diagnostic method | Based on symptoms after ruling out other possible causes[2][6] |
| Differential diagnosis | Wernicke–Korsakoff syndrome, delirium tremens, hypoglycemia, subdural hematoma, hyponatremia[1] |
| Treatment | Supportive care, treating triggers, lactulose, liver transplant[1][4] |
| Prognosis | Average life expectancy less than a year in those with severe disease[1] |
| Frequency | Affects >40% with cirrhosis[7] |
Hepatic encephalopathy (HE) is an altered level of consciousness as a result of liver failure.[2] Its onset may be gradual or sudden.[2] Other symptoms may include movement problems, changes in mood, or changes in personality.[2] In the advanced stages it can result in a coma.[4]
Hepatic encephalopathy can occur in those with acute or chronic liver disease.[4] Episodes can be triggered by infections, gastrointestinal bleeding, constipation, electrolyte problems, or certain medications.[5] The underlying mechanism is believed to involve the buildup of ammonia in the blood, a substance that is normally removed by the liver.[2] The diagnosis is typically based on symptoms after ruling out other potential causes.[2][6] It may be supported by blood ammonia levels, an electroencephalogram, or computer tomography (CT scan) of the brain.[4][6]
Hepatic encephalopathy is possibly reversible with treatment.[1] This typically involves supportive care and addressing the triggers of the event.[4] Lactulose is frequently used to decrease ammonia levels.[1] Certain antibiotics (such as rifaximin) and probiotics are other potential options.[1] A liver transplant may improve outcomes in those with severe disease.[1]
More than 40% of people with cirrhosis develop hepatic encephalopathy.[7] More than half of those with cirrhosis and significant HE live less than a year.[1] In those who are able to get a liver transplant, the risk of death is less than 30% over the subsequent five years.[1] The condition has been described since at least 1860.[1]
- ^ a b c d e f g h i j k Wijdicks, EF (27 October 2016). "Hepatic Encephalopathy". The New England Journal of Medicine. 375 (17): 1660–1670. doi:10.1056/NEJMra1600561. PMID 27783916.
- ^ a b c d e f g h "Hepatic encephalopathy". GARD. 2016. Archived from the original on 5 July 2017. Retrieved 30 July 2017.
- ^ a b "Hepatic encephalopathy". Clevelandclinic. Retrieved 9 June 2022.
- ^ a b c d e f Cash WJ, McConville P, McDermott E, McCormick PA, Callender ME, McDougall NI (January 2010). "Current concepts in the assessment and treatment of hepatic encephalopathy". QJM. 103 (1): 9–16. doi:10.1093/qjmed/hcp152. PMID 19903725.
- ^ a b Starr, SP; Raines, D (15 December 2011). "Cirrhosis: diagnosis, management, and prevention". American Family Physician. 84 (12): 1353–9. PMID 22230269.
- ^ a b c "Portosystemic Encephalopathy - Hepatic and Biliary Disorders". Merck Manuals Professional Edition. Retrieved 25 September 2019.
- ^ a b Ferri, Fred F. (2017). Ferri's Clinical Advisor 2018 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 577. ISBN 9780323529570. Archived from the original on 2017-07-30.